The place you call home might be influencing your health more than you realize, and there is research proving just how much. A cutting-edge practice known as geocoding is offering a new way to understand how where we live directly affects our well-being. By turning an address into geographic coordinates, researchers can map out health outcomes and link them to various communities and community characteristics. This breakthrough is shining a ligh t on how neighborhood factors like air quality, access to healthcare and local resources impact both adults and children—often in unexpected ways. To get the best healthcare possible to the right individuals in need, understanding the factors that go into their health is crucial.
For pediatric health, this research could be a game changer. If doctors could pinpoint communities where asthma, obesity or other chronic problems are more prevalent—simply by looking at where their patients live, the health concerns could be nipped in the bud. For instance, if a neighborhood shows high rates of respiratory problems or chronic illnesses, local health systems can act quickly, targeting interventions like improving air quality or building more health care facilities in the area. The research could also inspire further research into how geospatial tools could be used to inform other kinds of public health issues.
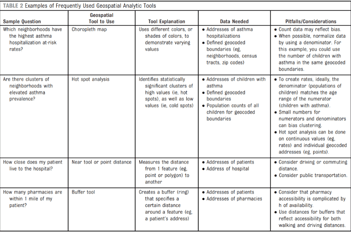
By using geocoding, healthcare providers can now see how certain types of environments—including everything from pollution to healthcare access—can shape the health of children. In a world where personalized healthcare is increasingly important, understanding these environmental factors is a crucial step in tailored care, especially for children in under-resourced areas. Moreover, recent studies have demonstrated that geospatial analysis, which includes tools like “hot spot analysis,” “choropleths maps” and “buffer tools”, can help healthcare providers identify said areas that have concerning health patterns. In this case one's environment includes community-level factors, community characteristics, or community social determinants of health.
What makes this approach even more powerful is the integration of these geographic insights into Electronic Medical Records (EMRs), something the research outlines. By combining environmental data with a child’s medical history, doctors can offer more personalized care that accounts for the unique challenges different children face in their respective neighborhoods. For example, researchers explain that a unique challenge could include, “a hospitalized patient living in an area with few, or low-quality, pharmacies [that] may benefit from receiving medications from an onsite pharmacy or by delivery.” (Tyris, et. Al, 2024) What makes this approach revolutionary is that it is not just about treating illnesses—it is about preventing them by understanding the environmental risks children are exposed to because of where they live.
That said, the potential of geocoding reaches utility beyond individual patients. By analyzing the geographic data of entire communities, health professionals can spot patterns that were once difficult to see. This would allow them to design interventions that target community-wide health disparities. This approach challenges the outdated notion of “one-size-fits-all" healthcare, where treatments and strategies are the same for everyone, regardless of where they live. In the words of the researchers, this research confirms geocoded health data as “truly a ‘sixth’ vital sign that should not be ignored. Knowing where [their] patients live facilitates [their] ability to visualize and contextualize [their] patients’ health with an understanding of their community and its characteristics.” (Tyris, et. Al, 2024)
At the heart of this research is a significant shift in the way some may think about healthcare. Instead of simply addressing medical conditions, healthcare providers are now considering the broader social and environmental factors that contribute to a child’s health. Some of the most significant beneficiaries could be the children living in under-resourced communities, who often face more challenges due to their environment.
This pioneering research is being driven by a team of experts at Children’s National, including Jordan Tyris, MD, MSHS, Gina Dwyer, MPH, Kavita Parikh, MD, MSHS, Anand Gourishankar, MBBS, MRCP, MAS, and Shilpa Patel, MD, MPH. Dr. Tyris and her team explain how knowing where a child lives allows doctors to gain a deeper understanding of the specific health challenges that a child faces, providing a more complete picture of their well-being.
The implications of this research are crucial to recognize. Geospatial analysis opens the door to a more equitable healthcare system, where interventions are not only based on individual conditions, but on the broader context of where patients live. By focusing on environmental factors, healthcare providers can target their resources more effectively ensuring that children from under-resourced areas have the same opportunities for good health as those in more privileged neighborhoods. The research could also inspire further research into how geospatial tools could be used to remedy other kinds of public health issues.
In a time when health disparities and privilege or lack thereof seem to be going hand in hand, personalized care seems to be the future. Understanding how our community characteristics impact our health is massively important. For children—especially those in under-resourced communities—this approach could mean a future with better access to care and a healthier tomorrow.
Related News
-

Training model improves autism knowledge among early childhood educators
February 17, 2026 -

In the News: FLiPRx “Food as Medicine” program boosts health for children and families
February 17, 2026 -
Welcoming pediatric hypertension expert Tammy M. Brady, MD, PhD to Children’s National
February 13, 2026