Children's National - NIAID Partnership

For each area, designated investigators from each institution are collaborating to design and conduct clinical research studies that will advance prevention strategies, diagnoses, treatments, and cures for the diverse range of pediatric diseases involving the immune system. Many of these studies will include children at high risk for complications related to their underlying disease or to experimental therapeutics and diagnostic tests they receive. Research participants will have the opportunity to be seen at both Children’s National and the NIH Clinical Center in Bethesda, Maryland. Together, the two institutions provide comprehensive, state-of-the-art pediatric clinical support, infrastructure, and research capacity. These resources protect the safety of children, ensure that they receive the highest quality of care, and offer them the opportunity to participate in cutting-edge clinical research. In addition, the partnership established joint training opportunities for physician-scientists interested in caring for these children while developing their research expertise in pediatric immunology, allergic, and infectious diseases.
News & Events
-
- Event
Children’s National Hospital – NIAID Symposium 2024
September 05, 2024


-
Protocol Title: Investigating the Mechanistic Biology of Immunodeficiency Disorders
Status: Recruiting
Project contact person: Stephanie Norman
This study investigates novel forms of primary immunodeficiency (PID) and to better define the natural history of both new and previously described forms of PID, including severe combined immunodeficiency (SCID), combined immunodeficiency, natural killer (NK) cell deficiency, and other disorders. Patients with clinical and/or laboratory evidence of PID will be recruited at Children's National and NIAID, and will provide one or more blood donations during the course of the study to enable immunologic and genetic investigations of immune pathways contributing to PIDs. These subjects will also be followed clinically to longitudinally assess the natural history of novel and known PIDs. Subjects will be followed over time with regard to their immunologic phenotype, clinical disease (including incidence of infections, autoimmune phenomena, allergic disease, or malignancies), and response to both preventative and definitive therapies. Biological relatives who do not have PID and healthy adult volunteers will also be eligible to serve as controls for this study.Children's National
 Michael Keller, MD, is a pediatric immunologist at Children's National Hospital and specializes in the diagnosis and treatment of primary and secondary immunodeficiency disorders. He has authored many peer-reviewed articles and contributed to expert consensus guidelines on the treatment and diagnosis of primary immunodeficiency disorders. Dr. Keller is a member of the American Academy of Allergy, Asthma, and Immunology (AAAAI); the Clinical Immunology Society; the European Society of Immunodeficiency; and the Primary Immunodeficiency Treatment Consortium (PIDTC).
Michael Keller, MD, is a pediatric immunologist at Children's National Hospital and specializes in the diagnosis and treatment of primary and secondary immunodeficiency disorders. He has authored many peer-reviewed articles and contributed to expert consensus guidelines on the treatment and diagnosis of primary immunodeficiency disorders. Dr. Keller is a member of the American Academy of Allergy, Asthma, and Immunology (AAAAI); the Clinical Immunology Society; the European Society of Immunodeficiency; and the Primary Immunodeficiency Treatment Consortium (PIDTC).Dr. Keller's research focuses on the use of adoptive T-cell therapies for treatment of infections in immunocompromised patients, including the use of this therapy to improve outcomes in children with primary immunodeficiency disorders as well as those undergoing bone marrow transplantation for cancer. He is the primary investigator of several Phase I-II studies of virus-specific T-cell immunotherapy.
NIAID
 Luigi D. Notarangelo, MD, received his medical degree from the University of Pavia, Italy. After completing training in pediatrics, subspecialty training in allergy/immunology, and human genetics at the University of Pavia and a postdoctoral internship with David Nelson, MD, at the Metabolism Branch, National Cancer Institute, he was appointed associate professor and subsequently full professor of pediatrics at the University of Brescia, Italy, where he chaired the department of pediatrics between 2000 and 2006. In November 2006, he joined the division of immunology at Boston Children’s Hospital, Harvard Medical School, as professor of pediatrics. In October 2016, he joined the Laboratory of Host Defenses.
Luigi D. Notarangelo, MD, received his medical degree from the University of Pavia, Italy. After completing training in pediatrics, subspecialty training in allergy/immunology, and human genetics at the University of Pavia and a postdoctoral internship with David Nelson, MD, at the Metabolism Branch, National Cancer Institute, he was appointed associate professor and subsequently full professor of pediatrics at the University of Brescia, Italy, where he chaired the department of pediatrics between 2000 and 2006. In November 2006, he joined the division of immunology at Boston Children’s Hospital, Harvard Medical School, as professor of pediatrics. In October 2016, he joined the Laboratory of Host Defenses.Dr. Notarangelo is a leader in the study of the molecular and cellular mechanisms of human primary immune deficiencies and in the treatment of these disorders. He has served as president of the European Society for Immune Deficiencies and of the Clinical Immunology Society. He has received numerous national and international awards.
 Ottavia Delmonte, MD, is the Assistant Research Physician of the Clinical Immunology and Microbiology Laboratory at NIAID.
Ottavia Delmonte, MD, is the Assistant Research Physician of the Clinical Immunology and Microbiology Laboratory at NIAID. -
Protocol Title: Natural History and Mechanistic Investigation of Atopic Disease in Childhood
Status: Recruiting.
Project contact person: Stephanie Norman
The prevalence of atopic diseases has increased both in developed and developing countries in recent decades. Atopic diseases typically manifest in early childhood, progress through the first decade of life through what has become known as the ‘atopic march’ and then often persist throughout one’s lifetime. This study will investigate the natural history of atopic diseases, including food allergies and asthma, to better understand the risk factors, predictors, and mechanisms underlying these diseases. Samples will be collected from patients with some form of atopic disease as well as healthy controls, for ex vivo analysis and in vitro experiments.
Children's National
 Hemant Sharma, MD, MHS, is the chief of the Division of Allergy and Immunology at Children’s National. He is an associate professor of pediatrics at George Washington University School of Medicine, and the director of the Food Allergy Program at Children’s National. He has served as the site director of the allergy immunology fellowship program with the National Institutes of Health. He is director of the FARE (Food Allergy Research & Education) Clinical Network site at Children’s National.
Hemant Sharma, MD, MHS, is the chief of the Division of Allergy and Immunology at Children’s National. He is an associate professor of pediatrics at George Washington University School of Medicine, and the director of the Food Allergy Program at Children’s National. He has served as the site director of the allergy immunology fellowship program with the National Institutes of Health. He is director of the FARE (Food Allergy Research & Education) Clinical Network site at Children’s National.He joined the faculty at Children’s National in 2008. His areas of clinical, advocacy and research interest include racial and socioeconomic health disparities and community-based management of food allergy. He writes a quarterly column in Allergic Living magazine and answers readers’ food allergy questions. He is heavily involved in advocacy, participating in regional and national legislative efforts to improve the health of the food allergy community. Dr. Sharma is board-certified in Pediatrics and in Allergy and Immunology, and is a fellow of the American Academy of Allergy, Asthma and Immunology, serving on the Adverse Reactions to Foods Committee. Due to his efforts on behalf of the food allergy community, he was selected to receive the 2016 FARE Vision Award.
 William Sheehan, MD, is a board-certified allergist and immunologist. He earned his medical degree from the Northwestern University Feinberg School of Medicine and a Bachelor of Arts degree from the College of the Holy Cross. Dr. Sheehan completed pediatrics internship and residency programs at the Duke University Medical Center before joining the Children’s Hospital of Boston Fellowship Program in Allergy and Immunology. He joined Children’s National Hospital in August 2017.
William Sheehan, MD, is a board-certified allergist and immunologist. He earned his medical degree from the Northwestern University Feinberg School of Medicine and a Bachelor of Arts degree from the College of the Holy Cross. Dr. Sheehan completed pediatrics internship and residency programs at the Duke University Medical Center before joining the Children’s Hospital of Boston Fellowship Program in Allergy and Immunology. He joined Children’s National Hospital in August 2017.Dr. Sheehan finds joy in helping patients with asthma, allergies, eczema and immunodeficiency. When not seeing patients, he is active in clinical research on asthma and allergies. He has spent much of his career investigating the interaction of environmental exposures and asthma. Dr. Sheehan's work has focused on improving the lives of inner-city children by eliminating detrimental exposure and improving health outcomes. With his expertise, he has assisted on several multi-center national asthma research networks. Additionally, Dr. Sheehan has recently been involved in two groundbreaking asthma prevention trials.
NIH
 Pamela Guerrerio, MD, PhD, graduated with a B.S. degree in biology from the University of Iowa and entered the Medical Scientist Training Program at Johns Hopkins University, where she completed medical school and a Ph.D. in human genetics. She also did her residency in pediatrics and fellowship in allergy and immunology at Johns Hopkins, and subsequently joined the faculty. In 2014, Dr. Guerrerio was recruited to the NIAID intramural research program as Chief of the Food Allergy Research Unit. She received tenure in 2019 and was named Chief of the Laboratory of Allergic Diseases in 2020. Dr. Guerrerio was the recipient of the ARTrust Faculty Development Award from the American Academy of Asthma, Allergy and Immunology in 2011. She received the Presidential Early Career Award for Scientists and Engineers, the National Science Foundation’s highest honor for science and engineering professionals in the early stages of their independent research career, in 2017.
Pamela Guerrerio, MD, PhD, graduated with a B.S. degree in biology from the University of Iowa and entered the Medical Scientist Training Program at Johns Hopkins University, where she completed medical school and a Ph.D. in human genetics. She also did her residency in pediatrics and fellowship in allergy and immunology at Johns Hopkins, and subsequently joined the faculty. In 2014, Dr. Guerrerio was recruited to the NIAID intramural research program as Chief of the Food Allergy Research Unit. She received tenure in 2019 and was named Chief of the Laboratory of Allergic Diseases in 2020. Dr. Guerrerio was the recipient of the ARTrust Faculty Development Award from the American Academy of Asthma, Allergy and Immunology in 2011. She received the Presidential Early Career Award for Scientists and Engineers, the National Science Foundation’s highest honor for science and engineering professionals in the early stages of their independent research career, in 2017. -
Protocol Title: Characterization of Pediatric Lyme Disease: Clinical Manifestations, Long Term Outcome, Immune Response, and Prevalence of PTLDs
Status: Substudy 1 - completed. Substudy 2 – not yet recruiting.
Project contact person: Stephanie Norman
The protocol proposes two paired substudies designed to characterize the clinical manifestations and long-term outcomes among pediatric Lyme disease patients in the greater Washington, DC area. Substudy 1 will characterize the natural history and longterm clinical, quality of life, and cognitive outcome of pediatric patients diagnosed with early and late stage Lyme disease, including prevalence of Post-Treatment Lyme Syndrome (PTLDS) and Substudy 2 will compare clinical, behavioral, cognitive and(future) immunologic response profiles between patients with full recovery, PTLDS and healthy controls. We will assess timeframe for resolution of symptoms after appropriate treatment, estimate the prevalence of PTLDS among a diverse cohort of pediatric patients diagnosed with Lyme disease within the past decade, and obtain specimens for future studies to identify the immune response of patients with PTLDS compared to patients who fully recovered from Lyme disease and healthy controls, as well as recently diagnosed patients with different manifestations of Lyme disease (early localized, disseminated, and late disease). Results of these analyses will be used to identify profiles and biomarkers that correlate with the outcome phenotypes. This signature could allow the design of a prognostic/diagnostic biomarker assays for patients with Lyme disease and PTLDS.
Children's National
 Roberta L. DeBiasi, MD, MS, is chief of the Division of Pediatric Diseases and co-director of the Congenital Zika Program at Children’s National Hospital. She holds appointments as tenured professor of pediatrics and microbiology, immunology and tropical medicine at George Washington University School of Medicine & Health Sciences as well as principal investigator in the Center for Health Outcomes Research & Delivery Science at Children’s National Research Institute. Dr. DeBiasi’s research expertise includes basic science as well as clinical/translational research. She serves as Principal Investigator for research and clinical trials focusing on severe and emerging viral infections affecting pregnant women, neonates, immunocompromised hosts, and normal children. She is co-director of the Congenital Zika Program at Children's National which includes research protocols in the US and Colombia focused on prenatal imaging, testing, genetics and virologic aspects of congenital Zika infection. She leads the Children's National Ebola response and is co-PI for federal funding to support Ebola preparedness. In addition, Dr. DeBiasi’s research portfolio includes a study evaluating the burden of pediatric Lyme disease, as well as long-term outcomes of Lyme infection in children. She is also involved in emergency investigational new drug (IND) acquisition of agents for treatment of severe viral myocarditis, encephalitis, and malaria. She is site PI for a PCORI- funded multicenter clinical trial evaluating optimal management of refractory Kawasaki Disease.
Roberta L. DeBiasi, MD, MS, is chief of the Division of Pediatric Diseases and co-director of the Congenital Zika Program at Children’s National Hospital. She holds appointments as tenured professor of pediatrics and microbiology, immunology and tropical medicine at George Washington University School of Medicine & Health Sciences as well as principal investigator in the Center for Health Outcomes Research & Delivery Science at Children’s National Research Institute. Dr. DeBiasi’s research expertise includes basic science as well as clinical/translational research. She serves as Principal Investigator for research and clinical trials focusing on severe and emerging viral infections affecting pregnant women, neonates, immunocompromised hosts, and normal children. She is co-director of the Congenital Zika Program at Children's National which includes research protocols in the US and Colombia focused on prenatal imaging, testing, genetics and virologic aspects of congenital Zika infection. She leads the Children's National Ebola response and is co-PI for federal funding to support Ebola preparedness. In addition, Dr. DeBiasi’s research portfolio includes a study evaluating the burden of pediatric Lyme disease, as well as long-term outcomes of Lyme infection in children. She is also involved in emergency investigational new drug (IND) acquisition of agents for treatment of severe viral myocarditis, encephalitis, and malaria. She is site PI for a PCORI- funded multicenter clinical trial evaluating optimal management of refractory Kawasaki Disease.NIAID
 Adriana Marques, MD, is the chief of the Lyme Disease Studies Unit, Laboratory of Clinical Immunology & Microbiology at the NIAID.
Adriana Marques, MD, is the chief of the Lyme Disease Studies Unit, Laboratory of Clinical Immunology & Microbiology at the NIAID.
Protocol Title: Pediatric SARS-CoV-2 and MIS-C Long-term Follow-up Study
Status: Active, not recruiting.
Project contact person: Saira Huq, [email protected]The protocol is a multisite prospective observational study to evaluate the clinical sequelae of symptomatic and asymptomatic severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection in the pediatric population, including coronavirus disease 2019 (COVID-19) and multisystem inflammatory syndrome in children (MIS-C), and characterize the immune response associated with these clinical presentations. Participants aged 21 years and younger with laboratory confirmed history of symptomatic or asymptomatic SARS-CoV-2 infection will visit the study sites for clinical and research evaluations and sample collection at schedules dependent on time since infection. Participants enrolled within 12 weeks after acute infection or positive test will be part of the “recovery group” and will attend study visits at baseline, every 3 months for the first 6 months, and subsequently every 6 months for a total of 3 years. Participants enrolled more than 12 weeks after acute infection or positive test will be in the “convalescent group” and will attend study visits at baseline and subsequently every 6 months for a total of 3 years.
Individuals (aged ≤21 years) without a diagnosis of SARS-CoV-2 infection or current symptoms suggestive of COVID-19 will serve as a control group and will attend visits for evaluations and sample collection at baseline and every 12 months for a total of 3 years. This protocol will establish a cohort of pediatric patients recovered from SARS CoV-2 infection and a biorepository for evaluation of the potential roles of host genetics, immune response, and other possible factors influencing long-term outcomes.
Children's National
NIAID
-
Protocol Title: Natural History Study of Pediatric-Onset Neuro-Immune Conditions with Discovery of Dysregulated Molecular And Genetic Pathways (NI-MAP)
Status: Recruiting.
Project contact person: Stephanie Norman
A natural history protocol for the evaluation of patients with genetically defined or undifferentiated pediatric diseases characterized by inflammation of the central nervous system using advanced genetics and immunophenotyping is currently being developed. Affected participants will be clinically evaluated and provide biological samples for research. Leftover samples from clinical procedures may also be used for research. Genotyping, HLA typing and immunophenotyping will be performed free of charge. Follow-up visit may be scheduled on the basis of clinical status, with the aim of molecularly characterizing biologic samples including CSF in both active and quiescent states. Unaffected biological parents will provide biological samples to be used as controls.
Children's National
 Elizabeth Wells, MD, is a graduate of Harvard University and the George Washington University School of Medicine and Health Sciences. She holds a master’s in Health Science from the NIH/Duke Clinical Research Training Program. Dr. Wells completed her pediatrics and neurology training at Children’s National Hospital and has been on staff as a pediatric neurologist within the Brain Tumor Institute and the Division of Neurology for the past 10 years.
Elizabeth Wells, MD, is a graduate of Harvard University and the George Washington University School of Medicine and Health Sciences. She holds a master’s in Health Science from the NIH/Duke Clinical Research Training Program. Dr. Wells completed her pediatrics and neurology training at Children’s National Hospital and has been on staff as a pediatric neurologist within the Brain Tumor Institute and the Division of Neurology for the past 10 years.In addition to her work in neuro-oncology at Children’s National, Dr. Wells also developed the multidisciplinary program in pediatric neuro-immunology. She serves on numerous national committees and receives national and international referrals for children with neuro-inflammatory disorders. She is a principal investigator for translational research studies and serves in a leadership role for the Clinical and Translational Science Institute at Children's National and the District of Columbia Intellectual and Developmental Disabilities Research Center. Dr. Wells has been director of Inpatient Neurology and the Neuroscience medical unit director since 2015 and was elected president of the medical staff in July 2020. In her role as vice president, Dr. Wells focuses on the programmatic development of the Center including work on quality and safety, medical informatics, diversity and inclusion and patient experience.
 Ilana Kahn, MD, is the clinical director of Neuroimmunology and the director of the Pediatric Multiple Sclerosis Options at Children's National Hospital.
Ilana Kahn, MD, is the clinical director of Neuroimmunology and the director of the Pediatric Multiple Sclerosis Options at Children's National Hospital.NIAID
 Raphaela T. Goldbach-Mansky, MD, MHS, received her medical degree from the University Witten-Herdecke, Germany, in 1990 and completed a combined residency in internal medicine and pediatrics at Case Western Reserve University, Metro Health Medical Center. She completed her rheumatology fellowship training at NIAMS in 1999 and served as a staff clinician at NIAMS through 2008. Dr. Goldbach-Mansky is chief of the NIAID Translational Autoinflammatory Disease Studies (TADS) Unit. She leads the NIAID autoinflammatory disease clinic and has built a translational research program focusing on clinical and translational studies in children with early-onset autoinflammatory diseases. Together with Dr. Daniel Kastner (NHGRI) she founded the Translational Autoinflammatory Research Initiative (TARI) at NIH to improve research in patients with rare autoinflammatory diseases.
Raphaela T. Goldbach-Mansky, MD, MHS, received her medical degree from the University Witten-Herdecke, Germany, in 1990 and completed a combined residency in internal medicine and pediatrics at Case Western Reserve University, Metro Health Medical Center. She completed her rheumatology fellowship training at NIAMS in 1999 and served as a staff clinician at NIAMS through 2008. Dr. Goldbach-Mansky is chief of the NIAID Translational Autoinflammatory Disease Studies (TADS) Unit. She leads the NIAID autoinflammatory disease clinic and has built a translational research program focusing on clinical and translational studies in children with early-onset autoinflammatory diseases. Together with Dr. Daniel Kastner (NHGRI) she founded the Translational Autoinflammatory Research Initiative (TARI) at NIH to improve research in patients with rare autoinflammatory diseases.Dr. Goldbach-Mansky's research focus is on applying a systematic approach to the clinical and immunological study of autoinflammatory diseases. Her group uses targeted interventions to understand the role of specific inflammatory pathways in the pathogenesis of autoinflammatory diseases.
 Bibi Bielekova, MD, received an MD in 1993 from Comenius University in Bratislava, Slovakia. After a medical internship at SUNY Downstate Medical Center in Brooklyn and a neurology residency at Boston University, she did a 3-year postdoctoral research fellowship at the NINDS Neuroimmunology Branch (NIB). She remained at NIB for an additional 5 years as a staff physician, focusing on development of novel therapies for MS. In 2005, she became associate professor of neurology with tenure and director of the Waddell Center for MS at University of Cincinnati. In 2008, she moved back to NINDS as an investigator. In 2018, Dr. Bielekova transferred as a senior investigator to NIAID. Her laboratory is studying mechanisms of immunoregulation and immune-mediated CNS tissue injury in MS and other neuroimmunological diseases with a long-term goal of developing effective therapies. In addition, Dr. Bielekova is a principal investigator on several innovative protocols including adaptively designed Phase I/II clinical trials.
Bibi Bielekova, MD, received an MD in 1993 from Comenius University in Bratislava, Slovakia. After a medical internship at SUNY Downstate Medical Center in Brooklyn and a neurology residency at Boston University, she did a 3-year postdoctoral research fellowship at the NINDS Neuroimmunology Branch (NIB). She remained at NIB for an additional 5 years as a staff physician, focusing on development of novel therapies for MS. In 2005, she became associate professor of neurology with tenure and director of the Waddell Center for MS at University of Cincinnati. In 2008, she moved back to NINDS as an investigator. In 2018, Dr. Bielekova transferred as a senior investigator to NIAID. Her laboratory is studying mechanisms of immunoregulation and immune-mediated CNS tissue injury in MS and other neuroimmunological diseases with a long-term goal of developing effective therapies. In addition, Dr. Bielekova is a principal investigator on several innovative protocols including adaptively designed Phase I/II clinical trials. -
One of the overarching goals of the CNH-NIAID partnership is to provide joint training opportunities for investigators studying and caring for children with infectious, immunologic, and allergic diseases. To date, 24 exceptional fellows have matched and been placed into the training programs. In 2020, a formal career mentorship program and a protocol writing workshop with program officers from the NIH Division of Allergy, Immunology, and Transplantation (DAIT) was initiated to better prepare fellows for careers in academic medicine.
Children's National
 Suzanne Kochis, MD, is the site director of the National Institute of Allergy and Infectious Diseases allergy and immunology fellowship program. She completed pediatric allergy immunology fellowship training at Johns Hopkins University. She obtained her MD from Jefferson Medical College of Thomas Jefferson University and then completed pediatric residency at Johns Hopkins, where she also served as Chief Resident. Her research at Hopkins focused on parental understanding of pediatric asthma control and outcomes for asthma, as well as a quality improvement project assessing adrenal insufficiency in patients with eosinophilic esophagitis on swallowed topical steroids. She now specializes in food allergies.
Suzanne Kochis, MD, is the site director of the National Institute of Allergy and Infectious Diseases allergy and immunology fellowship program. She completed pediatric allergy immunology fellowship training at Johns Hopkins University. She obtained her MD from Jefferson Medical College of Thomas Jefferson University and then completed pediatric residency at Johns Hopkins, where she also served as Chief Resident. Her research at Hopkins focused on parental understanding of pediatric asthma control and outcomes for asthma, as well as a quality improvement project assessing adrenal insufficiency in patients with eosinophilic esophagitis on swallowed topical steroids. She now specializes in food allergies.Dr. Kochis was the recipient of the American Academy of Pediatrics (AAP) Section on Allergy and Immunology (SOAI) Outstanding Abstract Award in 2017. She completed a Certificate in Quality, Patient Safety and Outcomes Research at the Johns Hopkins Bloomberg School of Public Health.
 Nada Harik, MD, is an attending physician in the Division of Infectious Diseases at Children's National Hospital in Washington, D.C and an associate professor of pediatrics at the George Washington University School of Medicine and Health Sciences.
Nada Harik, MD, is an attending physician in the Division of Infectious Diseases at Children's National Hospital in Washington, D.C and an associate professor of pediatrics at the George Washington University School of Medicine and Health Sciences.Dr. Harik is the director of the Pediatric Infectious Diseases Fellowship Program at Children's National. She also serves as the clinical consultant for the Infection Control Program. Her main research and clinical interests are Staphylococcus aureus epidemiology and pathogenesis, osteomyelitis/septic arthritis, infections in children with cystic fibrosis, infection prevention, tick-borne infections, medical student/resident/fellow education and pediatric tuberculosis. Dr. Harik is an active member of the Pediatric Infectious Diseases Society.
NIAID
 Paneez Khoury, MD, MHSc, FAAAAI, is an associate research physician at NIAID. She has been involved in translational research in eosinophilic disorders since joining the Human Eosinophil Section in 2012.She received her MD from University of Illinois College of Medicine in Chicago. She completed an internal medicine residency at the Ohio State University followed by a fellowship in allergy and clinical immunology at NIH. She also holds a master’s of health sciences from Duke University. She is board certified in internal medicine and allergy/immunology and is a fellow of the American Academy of Allergy, Asthma and Immunology (AAAAI).
Paneez Khoury, MD, MHSc, FAAAAI, is an associate research physician at NIAID. She has been involved in translational research in eosinophilic disorders since joining the Human Eosinophil Section in 2012.She received her MD from University of Illinois College of Medicine in Chicago. She completed an internal medicine residency at the Ohio State University followed by a fellowship in allergy and clinical immunology at NIH. She also holds a master’s of health sciences from Duke University. She is board certified in internal medicine and allergy/immunology and is a fellow of the American Academy of Allergy, Asthma and Immunology (AAAAI).At NIH, she serves as the chair of the Scientific Review Committee of the Laboratory of Parasitic Diseases. She sits on the graduate medical education (GME) committee, including the policy subcommittee, and is a member of the staff clinician council. Her external committee activities include involvement in the food allergy and eosinophilic disorders committee, the program directors assembly, and the leadership institute of AAAAI . She serves on the board of the International Eosinophil Society (IES) and is the social media chair for the society.
-
 Catherine Bollard, MD, MBChB, received her medical degree at the University of Otago in Dunedin, New Zealand. She is board certified both in pediatrics and hematology. She worked in New Zealand and London, England, before moving to Houston, Texas, in 2000 where she was a professor of pediatrics, medicine, and immunology at Baylor College of Medicine (BCM). In August 2013, she was recruited to Washington, D.C., to join Children’s National Hospital and George Washington University. She is currently the Bosworth Chair for Cancer Biology, director of the Center for Cancer and Immunology Research, and director of the Program for Cell Enhancement and Technologies for Immunotherapy (CETI) at Children’s National Hospital. She is a professor of pediatrics and of microbiology, immunology, and tropical medicine at George Washington University and the associate center director for translational research and innovation at the GW Cancer Center. Dr. Bollard is a member of the American Society for Clinical Investigation, is a past president of the International Society for Cellular Therapy, and the current president of the Foundation for the Accreditation of Cellular Therapy. She was a member of the Cellular, Tissues and Gene Therapies Advisory Committee of the FDA from 2015 to 2019 and, in 2019, became a member of the Frederick National Laboratory Advisory Committee for the NIH and an ad hoc member of the Pediatric Oncologic Drugs Advisory Committee for the FDA. She was an associate editor for the journal Blood from 2014-2021 and is currently editor in chief of Blood Advances. She has >200 peer reviewed publications and has been independently NIH funded for over 15 years. Her bench and translational research focuses on improving outcomes for patients after transplant and on the development of novel cell therapies for cancer and virus-associated diseases.
Catherine Bollard, MD, MBChB, received her medical degree at the University of Otago in Dunedin, New Zealand. She is board certified both in pediatrics and hematology. She worked in New Zealand and London, England, before moving to Houston, Texas, in 2000 where she was a professor of pediatrics, medicine, and immunology at Baylor College of Medicine (BCM). In August 2013, she was recruited to Washington, D.C., to join Children’s National Hospital and George Washington University. She is currently the Bosworth Chair for Cancer Biology, director of the Center for Cancer and Immunology Research, and director of the Program for Cell Enhancement and Technologies for Immunotherapy (CETI) at Children’s National Hospital. She is a professor of pediatrics and of microbiology, immunology, and tropical medicine at George Washington University and the associate center director for translational research and innovation at the GW Cancer Center. Dr. Bollard is a member of the American Society for Clinical Investigation, is a past president of the International Society for Cellular Therapy, and the current president of the Foundation for the Accreditation of Cellular Therapy. She was a member of the Cellular, Tissues and Gene Therapies Advisory Committee of the FDA from 2015 to 2019 and, in 2019, became a member of the Frederick National Laboratory Advisory Committee for the NIH and an ad hoc member of the Pediatric Oncologic Drugs Advisory Committee for the FDA. She was an associate editor for the journal Blood from 2014-2021 and is currently editor in chief of Blood Advances. She has >200 peer reviewed publications and has been independently NIH funded for over 15 years. Her bench and translational research focuses on improving outcomes for patients after transplant and on the development of novel cell therapies for cancer and virus-associated diseases. H. Clifford Lane, MD, serves as the National Institute of Allergy and Infectious Diseases' (NIAID) deputy director for Clinical Research and Special Projects. Dr. Lane's responsibilities include directing the activities of the Division of Clinical Research, which supports both intramural and extramural research involving human volunteers
H. Clifford Lane, MD, serves as the National Institute of Allergy and Infectious Diseases' (NIAID) deputy director for Clinical Research and Special Projects. Dr. Lane's responsibilities include directing the activities of the Division of Clinical Research, which supports both intramural and extramural research involving human volunteers -
 Jeffrey Dome, MD, PhD, is senior vice president of the Cancer and Blood Disorders Center at Children’s National Hospital in Washington, D.C. He also is professor of pediatrics at the George Washington University School of Medicine & Health Sciences and the Thomas Willson and Lenore Williams McKnew Professor of Pediatric Oncology. Dr. Dome received his medical degree from the University of Pennsylvania School of Medicine and his PhD degree in Medicine from Erasmus University in Rotterdam. He completed a residency in Pediatrics at Yale-New Haven Hospital and a fellowship in Pediatric Hematology/Oncology at Johns Hopkins Hospital. After fellowship, Dr. Dome was a faculty member at St. Jude Children’s Research Hospital before joining Children’s National Hospital in 2006. Dr. Dome is an internationally recognized expert on pediatric solid tumors, with an emphasis on kidney tumors and sarcomas. He chaired the Children’s Oncology Group (COG) Renal Tumor Committee, which oversees clinical research on kidney tumors at more than 200 children’s hospitals around the world, for more than 10 years. Dr. Dome is the Continental President of North America for the International Society of Paediatric Oncology (SIOP). He is a member of the Hematology/Oncology Sub board of the American Board of Pediatrics and serves on numerous medical advisory boards for cancer foundations. He has authored more than 150 articles, books and chapters on pediatric cancer.
Jeffrey Dome, MD, PhD, is senior vice president of the Cancer and Blood Disorders Center at Children’s National Hospital in Washington, D.C. He also is professor of pediatrics at the George Washington University School of Medicine & Health Sciences and the Thomas Willson and Lenore Williams McKnew Professor of Pediatric Oncology. Dr. Dome received his medical degree from the University of Pennsylvania School of Medicine and his PhD degree in Medicine from Erasmus University in Rotterdam. He completed a residency in Pediatrics at Yale-New Haven Hospital and a fellowship in Pediatric Hematology/Oncology at Johns Hopkins Hospital. After fellowship, Dr. Dome was a faculty member at St. Jude Children’s Research Hospital before joining Children’s National Hospital in 2006. Dr. Dome is an internationally recognized expert on pediatric solid tumors, with an emphasis on kidney tumors and sarcomas. He chaired the Children’s Oncology Group (COG) Renal Tumor Committee, which oversees clinical research on kidney tumors at more than 200 children’s hospitals around the world, for more than 10 years. Dr. Dome is the Continental President of North America for the International Society of Paediatric Oncology (SIOP). He is a member of the Hematology/Oncology Sub board of the American Board of Pediatrics and serves on numerous medical advisory boards for cancer foundations. He has authored more than 150 articles, books and chapters on pediatric cancer. Pamela Guerrerio, MD, PhD, graduated with a B.S. degree in biology from the University of Iowa and entered the Medical Scientist Training Program at Johns Hopkins University, where she completed medical school and a PhD in human genetics. She also did her residency in pediatrics and fellowship in allergy and immunology at Johns Hopkins, and subsequently joined the faculty. In 2014, Dr. Guerrerio was recruited to the NIAID intramural research program as Chief of the Food Allergy Research Unit. She received tenure in 2019 and was named Chief of the Laboratory of Allergic Diseases in 2020. Dr. Guerrerio was the recipient of the ARTrust Faculty Development Award from the American Academy of Asthma, Allergy and Immunology in 2011. She received the Presidential Early Career Award for Scientists and Engineers, the National Science Foundation’s highest honor for science and engineering professionals in the early stages of their independent research career, in 2017.
Pamela Guerrerio, MD, PhD, graduated with a B.S. degree in biology from the University of Iowa and entered the Medical Scientist Training Program at Johns Hopkins University, where she completed medical school and a PhD in human genetics. She also did her residency in pediatrics and fellowship in allergy and immunology at Johns Hopkins, and subsequently joined the faculty. In 2014, Dr. Guerrerio was recruited to the NIAID intramural research program as Chief of the Food Allergy Research Unit. She received tenure in 2019 and was named Chief of the Laboratory of Allergic Diseases in 2020. Dr. Guerrerio was the recipient of the ARTrust Faculty Development Award from the American Academy of Asthma, Allergy and Immunology in 2011. She received the Presidential Early Career Award for Scientists and Engineers, the National Science Foundation’s highest honor for science and engineering professionals in the early stages of their independent research career, in 2017. Pamela S. Hinds, RN, PhD, FAAN, is the director of the Department of Nursing Science, Professional Practice, and Quality, the William and Joanne Conway Endowed Chair in Nursing Research, and the research integrity officer at Children's National Hospital in Washington, D.C., and a professor of pediatrics at the George Washington University, School of Medicine and Health Sciences in Washington, D.C. She is an adjunct professor for the University of Pennsylvania, School of Nursing, Johns Hopkins University, School of Nursing, the University of Maryland, College of Nursing, and the Fudan University of Shanghai, China. For more than three decades, Dr. Hinds has created and led research related to the pediatric cancer experience, quality of life, fatigue and altered sleep during the treatment of pediatric cancers, and end-of-life communication and decision making. She has served on the Institute of Medicine (IOM) committee on end-of-life and palliative care for children in America (2003) and the National Quality Forum panel on palliative and end-of-life care in America, the Institute of Medicine (IOM) committee on Dying in America (2014) and is currently serving on the National Academies of Sciences, Engineering and Medicine Roundtable on Quality Care for People with Serious Illness (2016-2022), and the NCI Moonshot Tolerability Steering Committee (2019-present). Dr. Hinds is an Oncology Nursing Society Distinguished Nurse Researcher and the Association of Pediatric Oncology and Hematology Distinguished Nurse Researcher and is the Editor-in-Chief for the journal, CANCER NURSING: An International Cancer Journal and the open access journal, Cancer Care Research Online. She is the 2020 recipient of the HPNA Distinguished Nurse Researcher Award in Palliative Care and the 2020 Nightingale Award from the American Nurses Association and the Washington Post.
Pamela S. Hinds, RN, PhD, FAAN, is the director of the Department of Nursing Science, Professional Practice, and Quality, the William and Joanne Conway Endowed Chair in Nursing Research, and the research integrity officer at Children's National Hospital in Washington, D.C., and a professor of pediatrics at the George Washington University, School of Medicine and Health Sciences in Washington, D.C. She is an adjunct professor for the University of Pennsylvania, School of Nursing, Johns Hopkins University, School of Nursing, the University of Maryland, College of Nursing, and the Fudan University of Shanghai, China. For more than three decades, Dr. Hinds has created and led research related to the pediatric cancer experience, quality of life, fatigue and altered sleep during the treatment of pediatric cancers, and end-of-life communication and decision making. She has served on the Institute of Medicine (IOM) committee on end-of-life and palliative care for children in America (2003) and the National Quality Forum panel on palliative and end-of-life care in America, the Institute of Medicine (IOM) committee on Dying in America (2014) and is currently serving on the National Academies of Sciences, Engineering and Medicine Roundtable on Quality Care for People with Serious Illness (2016-2022), and the NCI Moonshot Tolerability Steering Committee (2019-present). Dr. Hinds is an Oncology Nursing Society Distinguished Nurse Researcher and the Association of Pediatric Oncology and Hematology Distinguished Nurse Researcher and is the Editor-in-Chief for the journal, CANCER NURSING: An International Cancer Journal and the open access journal, Cancer Care Research Online. She is the 2020 recipient of the HPNA Distinguished Nurse Researcher Award in Palliative Care and the 2020 Nightingale Award from the American Nurses Association and the Washington Post. Gina Montealegre, MD, is a physician scientist within the Division of Clinical Research, NIAID. She is a pediatric rheumatologist with a master's degree in Clinical Research. Dr. Montealegre has an extensive background in the development, execution and oversight of clinical trials in rare autoinflammatory diseases. Previously, she worked as a director of the Clinical Trials Unit at the Translational Autoinflammatory Disease Section at NIAID.
Gina Montealegre, MD, is a physician scientist within the Division of Clinical Research, NIAID. She is a pediatric rheumatologist with a master's degree in Clinical Research. Dr. Montealegre has an extensive background in the development, execution and oversight of clinical trials in rare autoinflammatory diseases. Previously, she worked as a director of the Clinical Trials Unit at the Translational Autoinflammatory Disease Section at NIAID. Luigi D. Notarangelo, MD, received his medical degree from the University of Pavia, Italy. After completing training in pediatrics, subspecialty training in allergy/immunology, and human genetics at the University of Pavia and a postdoctoral internship with David Nelson, MD, at the Metabolism Branch, National Cancer Institute, he was appointed associate professor and subsequently full professor of pediatrics at the University of Brescia, Italy, where he chaired the department of pediatrics between 2000 and 2006. In Nov. 2006, he joined the division of immunology at Boston Children’s Hospital, Harvard Medical School, as professor of pediatrics. In Oct. 2016, he joined the Laboratory of Host Defenses.
Luigi D. Notarangelo, MD, received his medical degree from the University of Pavia, Italy. After completing training in pediatrics, subspecialty training in allergy/immunology, and human genetics at the University of Pavia and a postdoctoral internship with David Nelson, MD, at the Metabolism Branch, National Cancer Institute, he was appointed associate professor and subsequently full professor of pediatrics at the University of Brescia, Italy, where he chaired the department of pediatrics between 2000 and 2006. In Nov. 2006, he joined the division of immunology at Boston Children’s Hospital, Harvard Medical School, as professor of pediatrics. In Oct. 2016, he joined the Laboratory of Host Defenses.Dr. Notarangelo is a leader in the study of the molecular and cellular mechanisms of human primary immune deficiencies and in the treatment of these disorders. He has served as president of the European Society for Immune Deficiencies and of the Clinical Immunology Society. He has received numerous national and international awards.
 David Wessel, MD, is executive vice president, chief clinical officer, physician-in-chief and the Ikaria Distinguished professor of Critical Care Medicine at Children's National Hospital. He is also professor of anesthesiology, critical care medicine and pediatrics at the George Washington University.
David Wessel, MD, is executive vice president, chief clinical officer, physician-in-chief and the Ikaria Distinguished professor of Critical Care Medicine at Children's National Hospital. He is also professor of anesthesiology, critical care medicine and pediatrics at the George Washington University.Dr. Wessel is internationally known for his pioneering work in caring for infants with heart disease. An experienced scientist and clinical researcher with more than 100 peer-reviewed publications, Dr. Wessel has designed and executed seminal studies in cardiac critical care and pulmonary hypertension; developed new therapies for perioperative care of the newborn with congenital heart disease and novel treatments of pulmonary hypertension; and studied neurologic outcomes relevant to perioperative care of newborns with congenital heart disease. He is a principal investigator and member of the steering committee for the Collaborative Pediatric Critical Care Research Network sponsored by the National Institutes of Health.
-
 Helen Kim, MBA, serves as the program director for the Children's National Hospital-National Institute of Allergy and Infectious Diseases partnership. She has a master’s degree in Business Administration from the Johns Hopkins Carey Business School. As program director, Helen provides leadership and oversight for all aspects of the collaborative partnership between the two institutions. Prior to joining Children's National, she was the senior clinical research program manager in the Department of Radiation Oncology and Molecular Radiation Sciences at Johns Hopkins.
Helen Kim, MBA, serves as the program director for the Children's National Hospital-National Institute of Allergy and Infectious Diseases partnership. She has a master’s degree in Business Administration from the Johns Hopkins Carey Business School. As program director, Helen provides leadership and oversight for all aspects of the collaborative partnership between the two institutions. Prior to joining Children's National, she was the senior clinical research program manager in the Department of Radiation Oncology and Molecular Radiation Sciences at Johns Hopkins.
-
 Stephanie Norman, MPH, joined the Children's National-NIAID partnership in July 2019 as the clinical research coordinator. She has a master's degree in public health from New York University. Prior to working at Children's National Hospital, she was a clinical research coordinator in maternal fetal medicine at Mount Sinai Hospital in New York City. As the coordinator for the partnership, she works on regulatory submissions, data entry, recruitment and enrollment as well as other tasks associated with daily protocol activity.
Stephanie Norman, MPH, joined the Children's National-NIAID partnership in July 2019 as the clinical research coordinator. She has a master's degree in public health from New York University. Prior to working at Children's National Hospital, she was a clinical research coordinator in maternal fetal medicine at Mount Sinai Hospital in New York City. As the coordinator for the partnership, she works on regulatory submissions, data entry, recruitment and enrollment as well as other tasks associated with daily protocol activity. Christine Peng, BSN, RN, is the research nurse for the Children's National-NIAID partnership. She received her BS degree in behavioral and community health from the University of Maryland, College Park, and BS in nursing from University of Maryland, Baltimore. Christine's roles within the partnership include providing education and support for the clinical research studies and functioning as a resource for the Principal Investigators, patient/family, and community.
Christine Peng, BSN, RN, is the research nurse for the Children's National-NIAID partnership. She received her BS degree in behavioral and community health from the University of Maryland, College Park, and BS in nursing from University of Maryland, Baltimore. Christine's roles within the partnership include providing education and support for the clinical research studies and functioning as a resource for the Principal Investigators, patient/family, and community.Infectious Disease Program: Pediatric SARS-CoV-2 and MIS-C Long-term Follow-up Study
 Saira Huq, MPH, is the project manager for the Pediatric SARS-CoV-2 and MIS-C Long-term Follow-up Study. She has a master of public health degree from the University of Pennsylvania and is a Fulbright Scholar. Prior to joining Children’s National, she helped evaluate federally funded public health programs and clinical trials at NORC at the University of Chicago and Westat. As project manager she coordinates study activities, monitors study progress, reports to the study sponsor, and helps ensure that project activities are completed on time, on budget, and within scope.
Saira Huq, MPH, is the project manager for the Pediatric SARS-CoV-2 and MIS-C Long-term Follow-up Study. She has a master of public health degree from the University of Pennsylvania and is a Fulbright Scholar. Prior to joining Children’s National, she helped evaluate federally funded public health programs and clinical trials at NORC at the University of Chicago and Westat. As project manager she coordinates study activities, monitors study progress, reports to the study sponsor, and helps ensure that project activities are completed on time, on budget, and within scope. Lauren Arrigoni, CPNP, RN, is the pediatric nurse practitioner (NP) for the Pediatric SARS-CoV-2 and MIS-C Long-term Follow-up Study with the Children's National-NIAID partnership. Her previous roles include pediatric heart transplant NP and Pediatric ICU nurse in NYC. At the height of the COVID-19 Pandemic in NYC in 2020, she was redeployed as a bedside nurse for the pediatric COVID-19 Unit and followed discharged COVID-19 pediatric patients as a part of the cardiology team.
Lauren Arrigoni, CPNP, RN, is the pediatric nurse practitioner (NP) for the Pediatric SARS-CoV-2 and MIS-C Long-term Follow-up Study with the Children's National-NIAID partnership. Her previous roles include pediatric heart transplant NP and Pediatric ICU nurse in NYC. At the height of the COVID-19 Pandemic in NYC in 2020, she was redeployed as a bedside nurse for the pediatric COVID-19 Unit and followed discharged COVID-19 pediatric patients as a part of the cardiology team.She is completing her doctor of nursing practice at the University of Pennsylvania. She obtained her BSN from the University of Pennsylvania as a Hillman scholar. While working full-time in the PICU, she graduated as a pediatric nurse practitioner from NYU where she was given the Rising Star Award. She also volunteers as a camp nurse at the Double H Ranch, which is a camp for children with serious and chronic illnesses, founded by Paul Newman. She has volunteered with MakerNurse, a group supporting nurse innovations and served as a guest of Doctor Radio on SiriusXM. Lauren’s roles within the study include conducting study visits, assessing study test results, and enrolling participants for the study.
 Mallory Barrix, MPH, CHES, joined the Children’s National-NIAID partnership in June 2021 as a clinical research coordinator on the Pediatric SARS-CoV-2 and MIS-C Long-term Follow-up Study. She has a bachelor of science in human development and family studies from the University of Wisconsin- Madison as well as a master of public health degree from Emory University. In addition, she is also a Certified Health Education Specialist. As a coordinator for the Pediatric SARS-CoV-2 and MIS-C Long-term Follow-up Study, she handles regulatory submissions, patient recruitment and enrollment, and study visit organization among other tasks aimed at helping the study run smoothly.
Mallory Barrix, MPH, CHES, joined the Children’s National-NIAID partnership in June 2021 as a clinical research coordinator on the Pediatric SARS-CoV-2 and MIS-C Long-term Follow-up Study. She has a bachelor of science in human development and family studies from the University of Wisconsin- Madison as well as a master of public health degree from Emory University. In addition, she is also a Certified Health Education Specialist. As a coordinator for the Pediatric SARS-CoV-2 and MIS-C Long-term Follow-up Study, she handles regulatory submissions, patient recruitment and enrollment, and study visit organization among other tasks aimed at helping the study run smoothly. Maureen Edu began working as a clinical research coordinator for the Pediatric SARS-CoV-2 and MIS-C Long-term Follow-up Study in January 2022. She assists with enrollment, recruitment, regulatory submission, data collection/entry, and other daily operations of the clinical study. She obtained her BS in biology from Randolph College. She formerly worked as a research coordinator for the Center for Prevention and Early Intervention at the Johns Hopkins Bloomberg School of Public Health.
Maureen Edu began working as a clinical research coordinator for the Pediatric SARS-CoV-2 and MIS-C Long-term Follow-up Study in January 2022. She assists with enrollment, recruitment, regulatory submission, data collection/entry, and other daily operations of the clinical study. She obtained her BS in biology from Randolph College. She formerly worked as a research coordinator for the Center for Prevention and Early Intervention at the Johns Hopkins Bloomberg School of Public Health. -
 7th Annual Symposium (Children’s National Research and Innovation Campus): September 5, 2024 | Learn more >
7th Annual Symposium (Children’s National Research and Innovation Campus): September 5, 2024 | Learn more >This annual symposium celebrates the partnership between Children’s National Hospital and the National Institute of Allergy and Infectious Diseases (NIAID). Established in 2017, the Children's National - NIAID partnership focuses on advancing the health of children with allergic, immunologic, and infectious diseases through collaborative research and education. Together with our co-host, the Pediatric Pandemic Network (PPN), it focused on "A New Paradigm: Infection-Associated Chronic Illnesses Affecting Children."
-
 6th Annual Children's National Hospital - NIAID Symposium (Children's National Research & Innovation Campus): April 27-28,2023 | Learn more >
6th Annual Children's National Hospital - NIAID Symposium (Children's National Research & Innovation Campus): April 27-28,2023 | Learn more >
This annual symposium celebrates the partnership between Children’s National Hospital and the National Institute of Allergy and Infectious Diseases (NIAID). Established in 2017, the Children's National - NIAID partnership focuses on advancing the health of children with allergic, immunologic, and infectious diseases through collaborative research and education. Together with our co-host, the Pediatric Pandemic Network (PPN), it focused on "Promoting Child Health: From Environmental Challenges to Pandemic."
-
 5th Annual Symposium (Virtual): June 2-3, 2022 | Recordings >
5th Annual Symposium (Virtual): June 2-3, 2022 | Recordings >
This two-day symposium brought together investigators, researchers, and clinicians from National Institute of Allergy and Infectious Diseases (NIAID) and Children’s National Hospital as well as other interested participants from outside institutions, and discussed the creation, progress, and evolution of this first-of-its-kind collaboration between the NIAID at the National Institutes of Health and Children's National, a leading pediatric health system in the Washington, D.C., area.
This year's symposium highlighted the current COVID-19 and Autoinflammatory/Neuroimmune diseases, with the onsite location at the Children’s National Research and Innovation Campus in DC. -
 4th Annual Symposium (Virtual): June 3-4, 2021 | Agenda > | Recordings >
4th Annual Symposium (Virtual): June 3-4, 2021 | Agenda > | Recordings >This annual symposium celebrates the partnership between Children’s National Hospital (CNH) and the National Institute of Allergy and Infectious Diseases (NIAID). Established in 2017, the CNH-NIAID partnership focuses on advancing the health of children with allergic, immunologic, and infectious diseases through collaborative research and education.
In 2021, the Symposium was held on Thursday, June 3rd and Friday, June 4th as a virtual event that highlighted research on COVID-19 and multisystem inflammatory syndrome in children (MIS-C), and the intersectionality of COVID-19, allergy, and immunology on the pediatric population. Keynote speaker pediatric neurologist and 73rd Governor of The Commonwealth of Virginia, Ralph Northam, spoke on the COVID-19 pandemic and strategies to reintroduce children into schools and sports.
-
 3rd Annual Symposium (Virtual): September 29, 2020 | Agenda > | Recordings >
3rd Annual Symposium (Virtual): September 29, 2020 | Agenda > | Recordings >
This year's symposium highlighted the latest COVID-19 and MIS-C pandemic, with a specific focus on the pediatric population. Dr. Anthony Fauci provided an overview on the infectious disease, and leading experts from Children's National, NIAID, and other institutions shared novel research and science being done to address this worldwide issue. -
 2nd Annual Symposium (NIH Natcher Conference Center | Bethesda, MD): November 8, 2019 | Agenda >
2nd Annual Symposium (NIH Natcher Conference Center | Bethesda, MD): November 8, 2019 | Agenda >
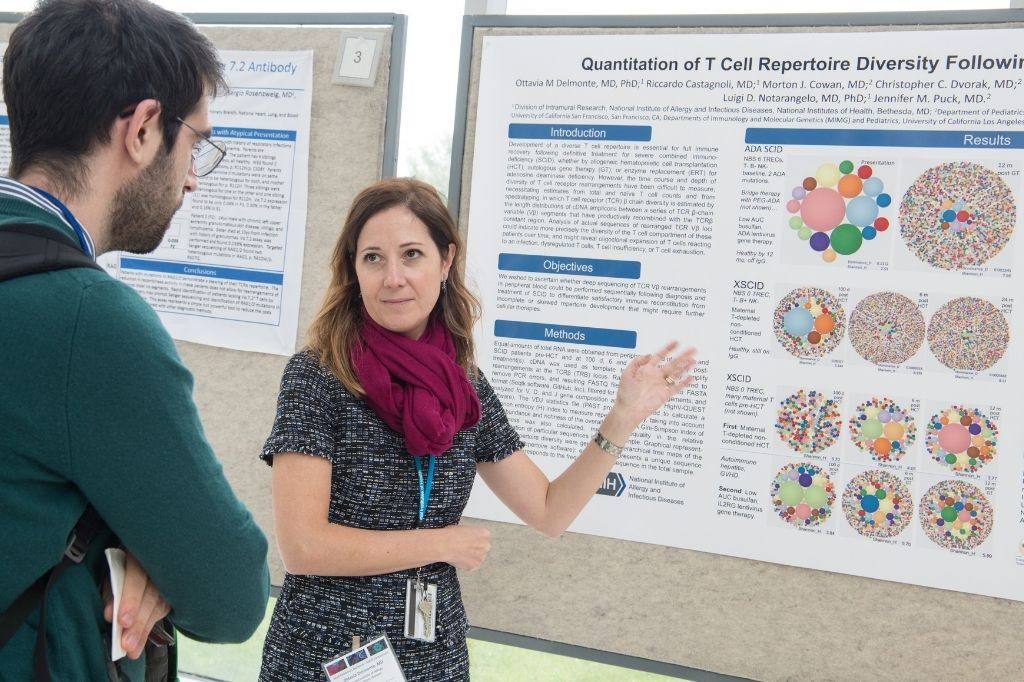
The 2nd annual Children’s National-NIAID Symposium presented outstanding research related to the partnership, including discussions on genomics, hereditary disorders, and gene therapies, by speakers from several NIH institutes and Children’s National, which included a poster session in the afternoon. Through this symposium, the partnership is committed to clinical and translational research and excellence in clinical care for children. -
 Inaugural Symposium (Children's National Hospital | Washington, DC): September 18, 2018 | Agenda >
Inaugural Symposium (Children's National Hospital | Washington, DC): September 18, 2018 | Agenda >
This one-day symposium brought together investigators, researchers, clinicians, and other interested participants from NIAID and Children’s National Hospital and discussed the creation, progress, and evolution of this first-of-its-kind collaboration between the NIAID at the National Institutes of Health and Children’s National Hospital, a pediatric academic medical center.
The symposium aimed to enhance knowledge and inspire present and future investigators to continue the search for innovative treatment approaches that will improve the lives of children with immunologic, allergic, auto-inflammatory, and infectious diseases.
