Cancer Biology and Experimental Cancer Therapy
Our Cancer Biology and Experimental Cancer Therapy research includes a focus on brain tumor biomarkers, led by Brian Rood, MD, Our Neurofibromatosis Research Group continues its work on the utility of MEK inhibitors (MEKi) in preventing the development of a variety of neurofibromatosis type 1 (NF1)-associated diseases. The D. Ashley Hill Laboratory focuses its research on the rare lung cancer known as pleuropulmonary blastoma (PPB).
Brain Tumor Biomarkers
Dr. Rood has created a Labeled Atlas of Medulloblastoma Proteins (LAMP) using stable isotope-labeled amino acids in culture (SILAC) technology. The LAMP has been used to quantitatively characterize the proteome of medulloblastoma subgroups to identify the functional pathways driving the disease.
In partnership with the Children’s Brain Tumor Tissue Collaboration, Dr. Rood is also applying proteomic techniques to identify novel genomic fusion events and disease specific protein isoforms creating tumor specific proteins. These proteins can serve as biomarkers, drug targets or neoantigens to be exploited for immunotherapy development. In collaboration with Harold Garner, PhD, of Virginia Tech, Dr. Rood has identified a panel of medulloblastoma-associated DNA microsatellite markers whose genotypes are non-randomly associated with tumor formation and can be used to differentiate those with the tumor based upon their germline DNA microsatellite variations.
Neurofibromatosis Program
The Neurofibromatosis Research Group, led by Yuan Zhu, PhD, continues their work on the utility of MEK inhibitors (MEKi) in preventing the development of a variety of neurofibromatosis type 1 (NF1)-associated diseases. Dr. Zhu and his team recently identified a therapeutic prospect in using a MEKi to prevent the formation of a developmental structural brain defect, an enlarged corpus callosum, which is also observed in a subset of NF1 patients with severe learning disabilities. Building on those results, the group has identified a similar therapeutic window during neonatal stages in which loss of NF1 leads to defects in both neuronal and glial precursors during cerebellar development. Importantly, MEKi treatment during the neonatal stage can rescue the developmental defects in the NF1-deficient cerebellum, providing a long-term benefit for motor function.
Together, those studies provide strong preclinical evidence that a single MEKi agent used during the early postnatal period can prevent the formation of developmental brain defects, providing long-term benefits for developing brain structures and developmental behaviors. To translate those preclinical findings to the clinic, the team completed an analysis of the brain penetration of the three MEKi compounds presently in clinical trials and presented the information to one of the leading industry partners sponsoring a MEKi clinical trial. Based on the team’s preclinical work and the ongoing clinical work of Roger Packer, MD, the Gilbert Family Neurofibromatosis Institute has agreed to open a third MEKi study, trametinib (Novartis), for children with NF1 and progressive brain lesions.
In addition, the team has used a series of genetic systems to identify the therapeutic window of NF1-related optic pathway gliomas (OPGs), which mainly occur in children younger than 7 years old with NF1.
Pleuropulmonary Blastoma (PPB)
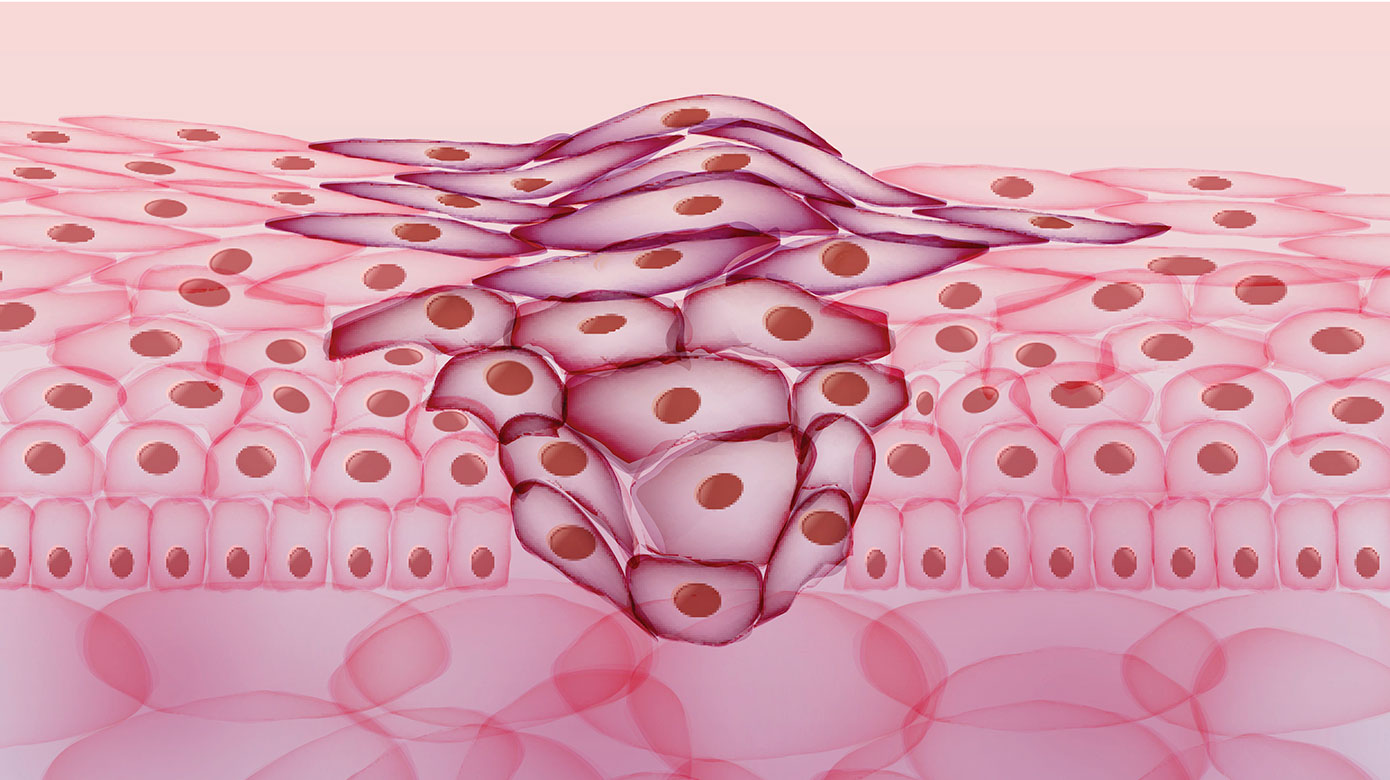
The Hill Laboratory has been devoted to clinical and genetic characterization of a cancer predisposition syndrome that features organ-based, embryonal cancers of children and adolescents, specifically the rare lung cancer pleuropulmonary blastoma (PPB). Through a linkage study, we identified germline mutations in the DICER1 gene as the basis of this cancer susceptibility, which is now known as DICER1 syndrome. Sequence analyses of PPBs and other syndromic tumors revealed a characteristic pattern of biallelic DICER1 mutations: one loss-of-function mutation (often inherited), and a second, tumor-specific missense mutation that always occurs in one of five “hotspot” codons within the RNase IIIb catalytic domain of DICER1. The resulting amino acid substitutions in the RNase IIIb domain of DICER1 protein disable proper cleavage of mature 5p miRNAs from their precursor (pre-miRNA) molecules. This miRNA deficiency results in extended expression of oncofetal genes beyond the normal developmental period and sets the stage for malignant transformation with additional genetic events, most prominently mutations or loss of TP53. Our laboratory is studying the effects of reconstitution of the key regulatory miRNAs and wild-type p53 function in tumors in vitro and in vivo; the latter using a cohort of patient-derived xenograft preclinical models.
The long-term goal of the research program is to develop safer and more effective management strategies and new, targeted therapeutics for DICER1 syndrome patients, and by extension, for childhood cancers more generally. In part, we accomplish this through continuing education of pediatricians and pathologists, and through improved methods for mutation-based screening to recognize syndromic neoplasias in their earliest stages, when they are most curable (Schultz et al Clin Cancer Res 2018). For the most threatening DICER1 syndrome cancers, such as advanced pleuropulmonary blastomas that were not diagnosed early, current chemotherapies are too often ineffective; about half of children with this disease die. We believe that new biologic or biomimetic therapies such as synthetic miRNA, other forms of oligonucleotide-mediated silencing for dysregulated oncofetal genes and corrective gene therapy (e.g., for TP53), will be effective if they can be properly targeted to tumor cells. This is a challenging problem, but our group has now developed tumor-derived cell lines and patient-derived xenograft preclinical models for some DICER1 syndrome cancers, in which new biologic agents and new methods for tumor-targeted delivery can be validated.
Finally, the Hill lab has a long-standing partnership with the International Pleuropulmonary Blastoma Registry (IPPBR), through which we strive to improve understanding of the molecular pathogenesis and clinical features of PPB, and to translate new knowledge into safer, more effective treatments. The IPPBR recently completed the first international prospective treatment study for PPB, which highlighted their capabilities for identifying and recruiting patients to clinical studies, and for establishing mutually beneficial relationships with pediatric oncologists around the world.
Faculty with Interests in Cancer Biology and Experimental Cancer Therapy

Jo Lynne Rokita, PhD
- Director, Brain Tumor Institute Bioinformatics Core
- Data Science Faculty