Blood Disorders
Investigators in this section are involved in the study of hematological, or blood disorder, diseases. We also research sickle cell disease, bleeding disorders and coagulopathy.
Hematology
Investigators in this section are involved in the study of hematological diseases, including:
- Treatment of patients with bleeding and clotting disorders.
- Understanding the varied phenotype and evaluating novel therapies for sickle cell disease.
- Improving the understanding of complications associated with blood transfusions.
Naomi Luban, MD, leads a team to investigate the adverse consequences of transfusion through epidemiological, clinical and device or laboratory methods development and evaluation. The multidisciplinary team works in concert with colleagues in:
- American Red Cross
- Children’s National Divisions:
- National Institute of Diabetes and Digestive and Kidney Diseases
- National Institutes of Health Division of Transfusion Medicine
- National Institutes of Health National Heart, Lung and Blood Institute
- U.S. Food and Drug Administration
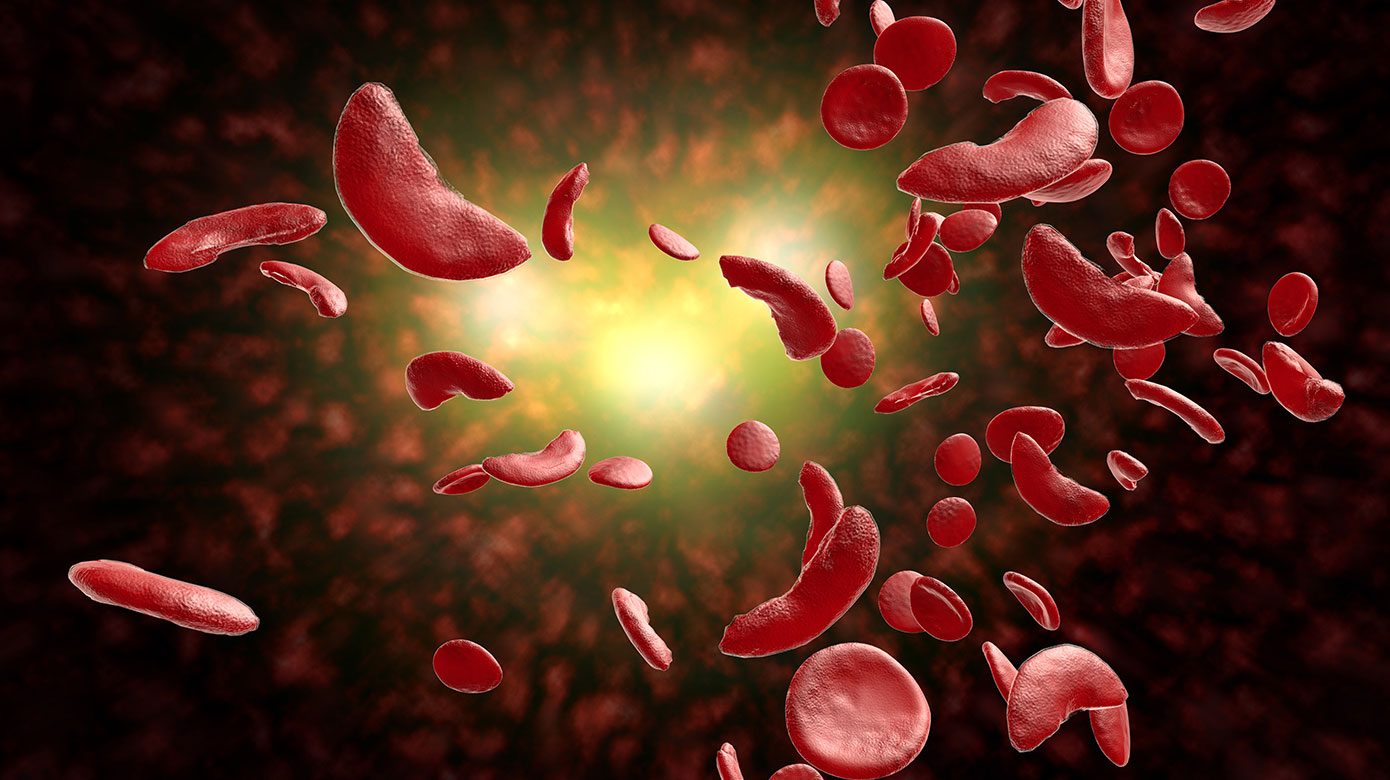
Sickle Cell Disease
Andrew Campbell, MD, focuses his research in understanding the varied phenotypic expression of sickle cell disease (SCD) in different populations through the CASiRe (Consortium for the Advancement of Sickle Cell Disease Research) international consortium, which he directs, including:
- Europe: Italy (University of Padova, University of Naples) and the United Kingdom (Guys St. Thomas)
- North America: six sites in the United States
- Africa: Ghana (Korle Bu Teaching Hospital)
The focus of the CASiRe Sickle Cell Research is the “CASiRe Renal Cohort Study” where they are describing the risk factors associated with proteinuria in different sickle cell populations within different ethnic groups, and also studying the role of the environment on the phenotype of sickle cell disease.
Dr. Campbell is also involved in industry-sponsored clinical trials in sickle cell disease, including the Voxelotor trial evaluating a novel small molecule drug that prevents the sickling of red blood cells.
Deepika Darbari, MD, is studying pain in SCD which is the most common complication of SCD. She is evaluating brain network connectivity patterns and its association with the burden of pain experienced by patients and investigating if these connectivity patterns can be used to evaluate therapies in sickle cell. She is also validating brain connectivity changes using electroencephalogram (EEG) in a NIH-funded study with a research group in Minnesota. Working with colleagues at NIH, Dr. Darbari has evaluated risk factors for persistent pain after reversal by hematopoietic stem cell transplant. Publications emerging from this work show for the first time the importance of non-hematological SCD factors in maintenance of pain in sickle cell disease after hematologic cure. Working with a multidisciplinary team including members of anesthesiology, pain psychology, palliative care and others at Children’s National, her team is testing feasibility of non-pharmacologic integrative therapies such as acupuncture in reducing pain burden in patients with SCD. She continues to serve on the Mayor’s Committee on newborn screening in the District of Columbia. More recently she has been invited to the committee (FDA and American Pain Society) tasked to develop guidelines for acute pain in sickle cell disease.
Hematologist Robert Nickel, MD, was recently awarded the prestigious Doris Duke Charitable Foundation’s inaugural Sickle Cell Disease/Advancing Cures Awards to advance curative approaches for sickle cell disease. The project is one of seven projects to win support for its potential to significantly improve the only current proven cure for sickle cell disease-hematopoietic cell transplantation. While transplantation using a matched sibling donor today has a high cure rate (greater than 90 percent) for sickle cell disease, traditional transplant approaches have many risks and side effects in both the short and long term. The study will examine if a chemotherapy-free approach can lead to a successful transplant without resulting in graft-versus-host disease (GVHD). GVHD is one of the most challenging complications of a transplant, in which the transplant immune cells attack the patient’s body. The researchers anticipate that this new transplant approach will be so well tolerated that patients’ quality of life will be maintained and improved throughout the process, with most of the care administered in a clinic setting.
In addition, Dr. Nickel is evaluating HLA antibody and platelet transfusions related to transplant for sickle cell disease with a Thrasher Research Fund Early Career Award. The primary aim of this study is to investigate if alloimmunization to class I HLA is associated with increased platelet transfusion requirements undergoing HLA-identical bone marrow transplant. He is also involved in a multi-center, NIH/NHLBI-funded grant to evaluate the real world implementation of the Stroke Prevention Trial in Sickle Cell Anemia (STOP) protocol in which transcranial Doppler (TCD), a measure of cerebral blood vessel velocity, is used to screen for stroke risk in children ages 2-16 with sickle cell disease.
Suvankar Majumdar, MD, is conducting research in electrocardiographic complications in sickle cell disease. This is an R01 funded joint PI project that evaluates the SCN5A gene and other genetic risk factors for prolonged QT and cardiac arrhythmias to understand why individuals with sickle cell disease are at higher risk of premature death. In addition, Dr. Majumdar is conducting an investigator-initiated phase 1/2 trial of intravenous citrulline, a powerful nitric oxide booster and vasodilator, as a novel intervention for the treatment of acute pain in sickle cell disease.
Naomi Luban, MD, continues her research on transfusion safety and methods to improve transfusion in sickle cell disease. She also chaired an NHLBI meeting whose publication in Transfusion is serving as the benchmark for future NIH and other funding for translational and clinical trials in transfusion in Neonatology and Pediatrics.
Bleeding Disorders and Coagulopathy
Michael Guerrera, MD, leads a multidisciplinary team working to improve the health of children and adolescents with bleeding disorders that is part of the Mid-Atlantic Region III Federally-Funded Hemophilia Treatment Centers. The team is currently involved in a number of clinical trials studying new products to treat and prevent bleeding in patients with hemophilia.
In addition, Dr. Guerrera and colleagues are involved in the American Thrombosis Hemostasis Network (ATHN) registries for bleeding and clotting disorders that is looking at inhibitor (antibody) risk from the newer agents. As part of the hemophilia regional network, investigators are looking at standardization and outcomes of surgery in patients with bleeding disorders and participating in the My Life Our Future project which involves genotyping patients and potential carriers with hemophilia A or B.
Yaser Diab, MD, has established complex anticoagulation assays to assist in the diagnosis and therapy of patients with thrombosis and those with the implantable Berlin Heart.
Drs. Diab and Guerrera hold multidisciplinary thrombosis clinics with the evaluation of demographic and outcome data on patients through a contract with the Centers for Disease Control and Prevention to improve therapy for children on Coumadin.