Rheumatology
Rheumatologic Disease Studies
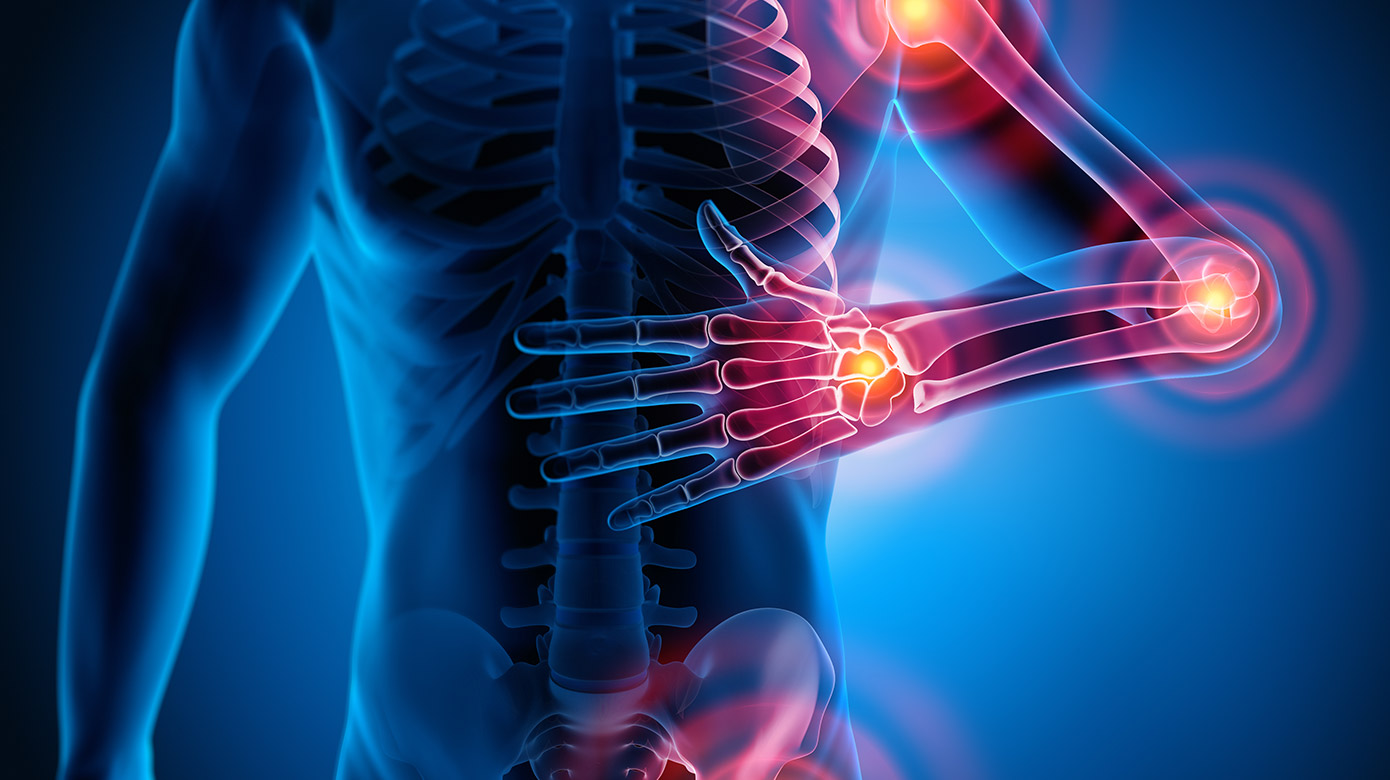
Our team conducts research surrounding pediatric rheumatologic diseases, including:
- Arthritis
- Dermatomyositis
- Granulomatous diseases
- Henoch-Schonlein purpura
- Kawasaki disease
- Lyme disease
- Musculoskeletal disease
- Multisystem inflammatory syndrome in children (MIS-C) associated with COVID-19
- Rheumatic fever
- Sjogren’s syndrome
- Systemic lupus erythematosus
- Scleroderma
Tova Ronis, MD, Research Areas
The Childhood Arthritis and Rheumatology Research Alliance (CARRA) at Children’s National is led by the site principal investigator, Tova Ronis, MD. This international collaborative research network seeks to understand pediatric rheumatologic diseases. The focus is on collecting physician and patient reported outcomes in a longitudinal study.
In 2020, the CARRA grant was awarded to Dr. Ronis to evaluate a tool to enhance training of the physical examination of the temporomandibular joint. Arthritis of the temporomandibular joint (TMJ) occurs in many juvenile idiopathic arthritis (JIA) patients. TMJ involvement in JIA can often be asymptomatic and difficult to detect. The effects of TMJ arthritis can have a severe impact on health-related quality of life that may persist into adulthood. Earlier detection and treatment should reduce joint damage and resulting facial deformity. Lack of standardization of the orofacial examination in JIA patients has made it difficult to study TMJ arthritis. Recently, a standardized orofacial physical examination protocol for JIA patients was published. The aim of the grant is to study the impact of using this protocol and a video training tool to see if it improves pediatric rheumatology fellows’ knowledge of TMJ arthritis and orofacial physical examination. This has the potential to improve clinical care by increasing detection of TMJ involvement in JIA patients which would prompt early treatment and prevent long term joint damage and deformity.
Dr. Ronis is also involved in the study of attitudes towards fertility in pediatric rheumatologic patients receiving cytotoxic therapy. The goal is to evaluate how teens and young adults with rheumatic disease feel about having their own children in the future. This has been done in teens with other conditions, but not in rheumatology patients.
Sangeeta Sule, MD, PhD, Research Areas
Our numerous industry-sponsored studies of treatments in juvenile idiopathic arthritis are spearheaded by Sangeeta Sule, MD, PhD. The goal of these studies is to evaluate the safety, efficacy and tolerability of treatment.
Dr. Sule is also involved in studying pain in children with rheumatologic autoimmune diseases. She is working with colleagues in anesthesiology to define signals to differentiate inflammatory pain from other causes. This is important because the prevalence of pain in children with rheumatologic autoimmune diseases is high. Pain negatively impacts outcomes including increased risk of anxiety, depression, decreased school performance and increased risk of unemployment in adults. The problem is that there is no single effective way to assess the type of pain (disease activity vs. amplified pain). Current methods are subjective and largely reflect intensity and may be hampered by overlying psychological factors such as depression. We need an effective way to assess baseline pain and response to pain with interventions. A biomarker for pain would mitigate problems associated with escalating drugs and serve to inform more precise treatment for both disease activity and pain.
Dr. Sule studies the effects of diet, exercise and nutrition on autoimmune disease. She has published on the negative effects of obesity and low physical activity in pediatric arthritis and lupus. Using large national databases, Dr. Sule has also shown that children with a history of juvenile arthritis have an increased risk of coronary artery disease into adulthood. She is starting a study of dietary habits and disease flare in children with lupus.

